Malpractice, misconduct history of military-employed doctors shielded by defense department
The DOD paid out nearly $1 billion in claims, but providers often show clean public disciplinary record
(InvestigateTV) — The surgery on the soldier’s son was supposed to be routine. But in a matter of minutes, the once-vibrant 1-year-old ZaMari Reese was fighting for his life.
When it was all said and done, a series of medical mistakes, misjudgments and miscalculations at a prestigious military hospital cost the toddler his quality of life, leaving him permanently brain-damaged and requiring round-the-clock care. His family won a malpractice case against some of the doctors involved.
Reese’s case is among the nearly $1 billion in malpractice claims that the U.S. Treasury has paid for mistakes made by members of the military medical community, according to an InvestigateTV analysis of judgment data reported annually to Congress.
The names of military medical personnel involved in malpractice claims or disciplined for errors are shrouded in secrecy by the Department of Defense.
Since 2022, InvestigateTV has been pressing the Defense Health Agency, the Defense Department arm in charge of military care, for the names of military medical personnel disciplined for misconduct and/or involved in malpractice claims.
After the threat of potential legal action, InvestigateTV received data from the Defense Health Agency that had never before been made public. It shows that since 2018, there have been at least 478 military medical providers reported by the Department of Defense to a confidential federal repository that contains information about disciplined doctors and medical malpractice judgments.
The names listed in the repository include both civilian and military medical providers and only are accessible to hospitals, state medical boards, and other entities making medical hiring decisions.
The data provided to InvestigateTV also shows that there have been:
- 160 suspensions of 30 days or more of military medical personnel between the middle of 2020 and 2022,
- Nearly 200 cases where military providers had action taken against their privileges to practice between 2018-2022,
- And more than 250 cases where peer review panels found military providers failed to meet the basic standard of care in that same five-year timeframe.
Yet the names of those providers remain hidden.

In the civilian world, the names of rogue doctors are readily accessible from state medical boards and through state court records. The military could take the same route, said Natalie Khawam, an attorney who has represented military members and their families in medical claims.
“There’s no law or act, as they say, that requires them to share this information. Does that need to change? Sure, it does. Just one more thing DOD should do. But they don’t need a law to do that. They could do it on their own. They could just provide this information,” Khawam said.
Malpractice cases cloaked in military secrecy include ZaMari Reese, the toddler injured during surgery.
‘After the incident, it showed me what the military really is’
When he came into the world in 2015, TimMeka Harris-Reese knew her son would be a handful. “He was a ball of fire from the beginning,” she said.
Little ZaMari was a force of nature in his tight-knit military family, the kind of baby who commanded everyone’s attention. Huggable. Chunky. Lovable. Those are the words used to describe him in his first year of life.
But 12 days after happily smashing his first birthday cake in front of friends and family, ZaMari Reese’s life took a drastic turn. Court records show that in September of 2016, his parents took him to Walter Reed National Military Medical Center in Maryland, the flagship military hospital known for treating U.S. presidents as well as service members and their families.
Then one-year-old ZaMari was supposed to get ear tubes, a procedure hundreds of thousands of kids have each year. He was also scheduled to have his adenoids removed, another common surgery for children.
It was all supposed to be quick and simple. It wasn’t.

Photos show ZaMari just out of surgery - connected to tubes, covered in cords, and in a coma. His parents were told he suffered a permanent brain injury caused by a lack of oxygen during surgery.
“His heart stopped, and he had coded on the table during surgery,” TimMeka Harris-Reese said. “I lost it because I just didn’t know what happened.”
Court records spell out the full story TimMeka and her husband, Army Staff Sgt. Douglas Reese, didn’t learn completely until days later.
Documents claim the couple was never warned that ZaMari, who has sickle cell and reactive airway disease, was at greater risk for complications or even death. The records claim an anesthesiologist working for the military was aware of the risk, repeatedly voicing concerns before and during ZaMari’s procedures.
Robert Michael, the family’s attorney, said despite the concern, military doctors proceeded with the surgeries. And their work continued even when there were clear indications that ZaMari was struggling to breathe and going into heart failure.
“There was a huge jumbotron in the corner that was displaying all of this. Alarms were going off for three different things. He wasn’t being ventilated properly. His respirations were off, and his blood pressure was off,” Michael said. “Midway through the operation, a fourth alarm started going off. All of which they ignored.”
A lawsuit filed against the federal government by the family in July of 2019 claims a resident physician handled the procedures with an attending physician supervising, something the Reeses said they were unaware of until after the damage had been done.
“I’m angry. I wish I never went through with that procedure. I mean, sometimes I feel like it’s my fault because I’m the one who took him back and laid him on that table,” Harris-Reese said.
Nearly 90 minutes after ZaMari was first given anesthesia, and with his vitals significantly declining, court records indicate one of the anesthesiologists finally intervened, telling the surgeons “You need to stop”, just before ZaMari’s heart did.
“The sad part about this case is this procedure could have been stopped at any moment with no harm to this child,” Michael said.
The harm for ZaMari is permanent. Now eight, he cannot walk or talk, is wheelchair-bound, and requires round-the-clock care from his mother just to keep him alive.

The family’s suit went to trial in 2022. The judge in the case ultimately ruled three of the military doctors involved in ZaMari’s case breached the standard of care and were medically negligent. The family was awarded millions of dollars specifically for the care he’ll need for the rest of his life.
“Even though the settlement is going to help ZaMari in the long run, no amount of money will replace what they took from my child. No amount of money,” said Harris-Reese.
The bittersweet victory won by the Reese family following their malpractice case is far from unique. InvestigateTV analyzed the numbers from an annual report made to Congress that details payments for malpractice claims against providers in the armed forces.
We found payments made in 67 cases just between January and September of 2023, totaling more than $80 million.
Since 2009, the data shows that nearly 1,500 claims have been paid because of mistreatment by military providers. Those claims cost taxpayers a stunning amount: almost $1 billion.
“That tells me there’s a very significant problem with military medicine that needs to be looked at and addressed. And it would start, in my mind, withholding these doctors and the other folks involved individually accountable for what’s happened here,” Michael said.

Military healthcare providers often shielded by secretive system when things go wrong
When it comes to holding military providers accountable, InvestigateTV discovered a secretive system that allows problematic doctors to remain largely in the shadows, protected from the financial and reputational cost that’s often faced by their civilian counterparts.
Malpractice claims related to cases involving military providers are paid by the U.S. Treasury Department. That annual report to Congress does not name the physicians or providers involved, whose information may only come to light when egregious cases make headlines or filings end up on the internet, as they did in the Reese case.
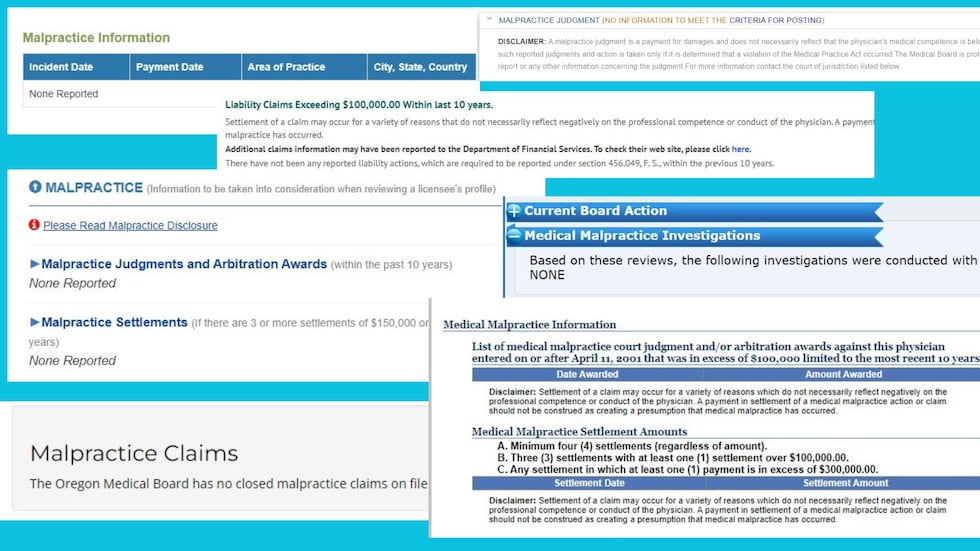
By contrast, in the civilian world, malpractice judgments are often included among the information provided openly by state medical boards. Physicians in the U.S. typically have a public profile page maintained by the state medical board that holds their license.
In many states including California, Florida, Georgia, Maryland, North Carolina, Oregon, and Texas, InvestigateTV found information about malpractice payments are included in those public internet profiles that anyone can access.
However, many military providers are protected behind a shield of secrecy.
Steve Ellis is president of Taxpayers for Common Sense, a government watchdog group. He believes the malpractice spending by the government raises big questions Congress should be asking, not only about transparency but also military health care quality.
“There’s no reason for the military to shield them. Right now, the secrecy isn’t really helping anyone except for people who are bad actors,” he said.
The Defense Health Agency reports malpractice claims and some forms of disciplinary action to state boards that license doctors. Then those boards decide based on their own investigations of the cases whether they’re made public.
InvestigateTV scoured hundreds of publicly available records from state medical boards across the country and found the reporting of discipline related to military providers is not widely seen.
The Federation of State Medical Boards, a lobbying group that represents medical boards across the nation, did not respond to specific questions from InvestigateTV about the public reporting of military discipline.
“There’s always a balancing act between privacy - whether it’s privacy for doctors, privacy for patients. But you can still get some level of data that isn’t going to hurt anybody’s privacy but is going to shed some light on the problem and the issue,” Ellis said. “The government should be putting this information out already. It’s just embarrassing.”

Defense Department fought attempts to unmask military physicians with malpractice or disciplinary history
InvestigateTV has been battling the Defense Health Agency and Department of Defense for nearly two years, trying to get information about doctors and other healthcare providers involved in military malpractice cases and disciplinary action.
Since May of 2022, our team has filed nine Freedom of Information Act requests with both departments as well as the individual branches of service with the goal of getting specific details about thousands of malpractice cases involving military practitioners.
For months InvestigateTV has pressed the agencies, consistently calling, and sending at least 60 emails following up. Despite being told early on that records would be provided, the requests have been repeatedly denied.
“You’re doing these stories to let everyone know the truth. And the DOD’s fighting you from letting you know the truth,” attorney Natalie Khawam said. “Why are they hiding it? Because it’s bad.”

Khawam has represented dozens of families who’ve filed malpractice claims or lawsuits related to military malpractice. Her work advocating to give active-duty service members the ability to file malpractice claims against the military was highlighted in a 2022 InvestigateTV report.
Before a change in federal law championed by Khawam and one of her clients, Army Sgt. Richard Stayskal, active-duty military members were essentially barred from filing malpractice claims because of legal precedent set decades ago.
However, that court decision did not apply to the spouses and children of service members injured or killed at the hands of military doctors and care providers, giving them the right to pursue compensation from the government – with only limited information released about their cases.
DHA data shines a light on disciplinary action against military providers
The data provided to InvestigateTV by the DHA also provides details about the number of military providers who’ve been subjected to disciplinary action that’s largely kept quiet. Since 2018 it shows that there have been hundreds of disciplinary actions, from suspensions to license restrictions.
Yet no one knows who these military healthcare providers are.

“It’s scary what is going on. Are they hiring cooks to do surgery? What is going on?” Khawam said after seeing the data. “How can you have that many incidents and that many problems and that much cost? And the scary part is, who are they?”
FOIA requests made by InvestigateTV asked for the names of military providers reported by the Defense Health Agency for malpractice payments or disciplinary action.
DHA failed to provide the names, but we’re continuing to fight, filing new requests for information. The DHA also declined InvestigateTV’s repeated requests for an interview.
In a statement, DHA officials acknowledged disciplinary actions are not made public by the military, providing little explanation as to why, other than citing federal code.
“Reporting determinations are part of the medical quality assurance program and are confidential and privileged pursuant to section 1102 of Title 10, United States Code and DHA may only release such information consistent with that statute,” the agency said in an email to InvestigateTV.
The DHA also failed to supply an expert to answer questions about the data on background, despite repeated requests.
InvestigateTV sent our findings to Congressional lawmakers on both sides of the aisle, some veterans themselves. None of them responded to requests for comment.
Attorney Robert Michael, the man representing the Reese family, said, “There’s really not a degree of accountability under the current military medicine system that there needs to be.”
He hopes shining a light on cases like the one involving ZaMari Reese will change that. But Michael knows many military families are reluctant to fight the government they risk their lives for - let alone talk about it.
“My husband put those boots on before my son’s injury and he continued to put those boots on after,” TimMeka Harris-Reese said.

Sgt. Reese recently retired from the Army after more than a decade of service. His wife continues soldiering on with the task of caring for their son. It’s a job that never stops, with ZaMari needing as many as 32 medications each day as well as diaper changes and monitoring for seizures his family says occur frequently.
TimMeka admits it’s exhausting work she never imagined she’d have to do for a child whose life had incredible promise. While she maintains her family does all it can to give ZaMari a good quality of life, she can’t help but feel angry at what’s been lost because of medical malpractice.
“At the end of the day we have to learn to forgive,” she said. “I won’t never forget.”
Associate producer Charlie Roth contributed research to this report
Have you experienced military medical malpractice? InvestigateTV would like to hear from you.
By clicking “Submit” you agree to our terms and conditions regarding your information and image in our Publicity Release and Copyright License, Terms and Conditions






